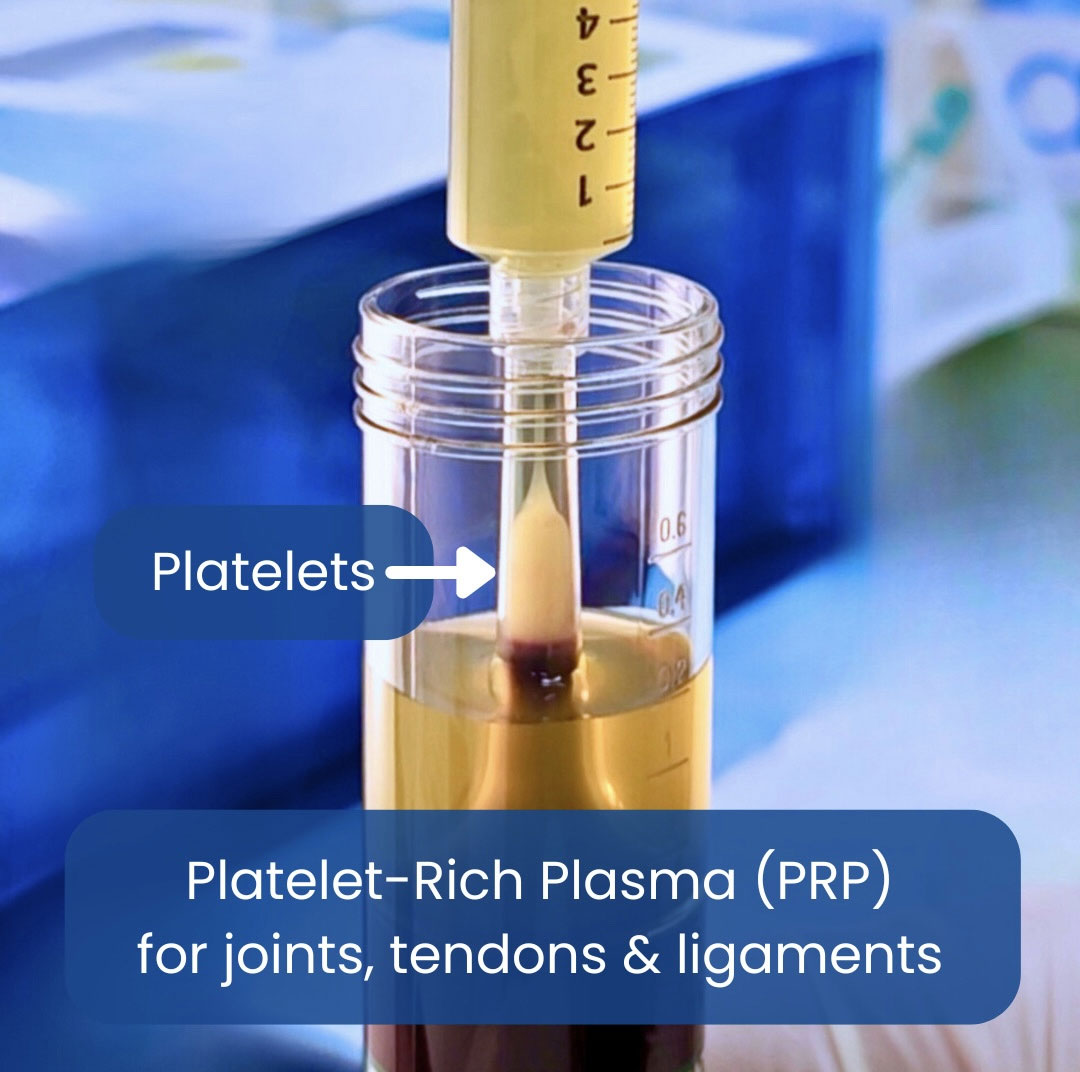
Why total platelet dose matters?
by Dr Ameer Ibrahim
Sport & Exercise Medicine Physician
Across recent syntheses and expert reviews, higher total platelet numbers delivered to the joint are associated with better clinical outcomes, particularly for function and durability of effect. The emerging consensus is shifting away from reporting only "×-fold concentration" toward absolute platelet dose (platelets delivered = PRP platelet concentration × injection volume).
(Source: arthroscopyjournal.org)
What the Newest Reviews Show (2024-2025)
Systematic Review (Arthroscopy/AJSM family, 2024-2025): Trials that reported greater platelet doses tended to show larger improvements in pain and function versus lower-dose PRP, suggesting dose is a key driver of efficacy rather than the label "PRP" alone. Editorials around this work directly argue platelet count should be specified and optimized.
(Source: arthroscopyjournal.org)Current Concepts Review (2024 PDF): Proposes a dose-response relationship with a provisional threshold >10 billion platelets per injection for favorable outcomes in KOA-effects more pronounced for function than pain.
(Source: SpringerLink)Network Meta-Analysis (2025): When PRP arms were stratified by dose, higher-dose regimens ranked better for key patient-reported outcomes, supporting a clinically meaningful advantage to delivering more total platelets. (Evidence limited by heterogeneity in preparation/reporting.)
(Source: BioMed CentralVery Recent Systematic Review (2025, in press): Reiterates that variability in platelet concentrations and total dose likely explains inconsistent findings across PRP trials and calls for standardized, dose-based reporting.
(Source: ScienceDirect)
How Much is "Enough"?
Numbers vary by study, but several converging signals have emerged:
- Minimum Effective Range: Some overviews suggest outcomes improve once total dose exceeds ~3.5-5 billion platelets, with better durability as doses rise.
(Source: MDPI) - Provisional "Optimal" Target: Multiple authors highlight ~10 billion platelets per injection as a pragmatic target associated with superior functional gains and possible chondroprotection, acknowledging the need for confirmatory RCTs.
(Source: SpringerLink) - Technique Note: Reaching "super-high" doses may require larger PRP volumes and/or double-spin protocols, which should be balanced against practicality and patient tolerance.
(Source: SAGE Journals)
Nuances & Caveats
- Heterogeneity remains high. Results are influenced by leukocyte content (LP-PRP often preferred for KOA), activation method, anticoagulant, spin protocol, baseline OA grade, and number/timing of injections-so dose is necessary but not the only variable.
(Source: SAGE Journals) - Pain vs Function. Dose effects appear stronger for functional scores (e.g., WOMAC function) than for pain alone-an important counseling point.
(Source: SpringerLink) - Comparators. Contemporary evidence still supports PRP (particularly higher-dose protocols) outperforming HA and often corticosteroid at 6-12 months, though study quality varies.
(Source: BioMed Central) - Reporting Gaps. Many trials still omit absolute platelet counts. Future studies are urged to standardize dose (total platelets) and cumulative dose across multi-injection series.
(Source: ScienceDirect)
Practical Takeaways for Clinics
- Ask for the numbers. Document baseline whole blood platelet count, PRP platelet concentration, injection volume, and thus total platelets delivered per injection. Ideally 30-60 ml of blood is needed per knee.
(Source: arthroscopyjournal.org) - Aim higher when feasible. For symptomatic KOA, consider targeting ~10 billion platelets per injection (or an equivalent cumulative dose across a short series), while tailoring to patient factors and device capabilities.
(Source: SpringerLink) - Standardize beyond dose. Prefer leukocyte-poor PRP, use consistent prep and injection schedules, and track outcomes at 3, 6, and 12 months.
(Source: SAGE Journals)
Bottom Line
The total platelet number delivered intra-articularly is emerging as a key determinant of PRP efficacy in knee OA. While exact cut-offs need high-quality, head-to-head RCTs, the weight of recent evidence favors higher platelet doses-on the order of several to ~10 billion platelets per injection-for more reliable, durable functional benefits. Standardized, dose-centric reporting will be essential to refine these targets.
